Tracking Data to Help Health Officials
Tuesday, November 17, 2020
When the COVID-19 pandemic broke out early this spring, three Carlson School faculty members found a distinctive way to contribute to the fight. Their weapon? Data.
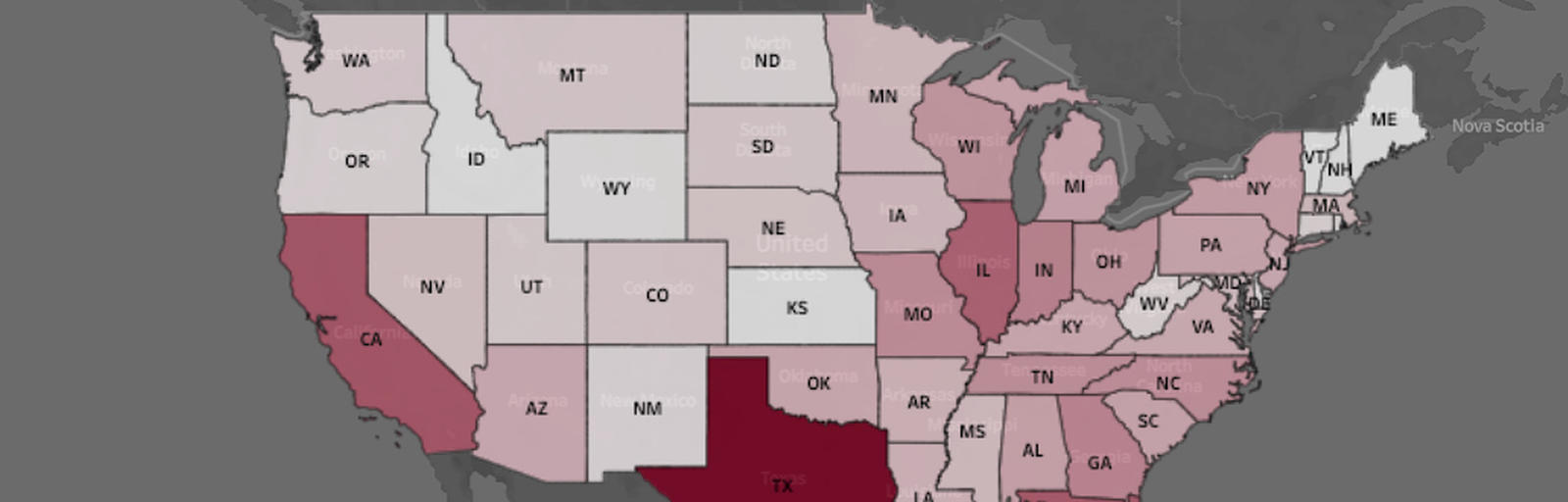
The COVID-19 Hospitalization Tracking Project is a collaborative effort between the two centers within the Carlson School: the Medical Industry Leadership Institute (MILI) and the Management Information Systems Research Center (MISRC). The project collects, tracks, and publicly reports daily COVID-19 hospitalizations from all 50 states and the District of Columbia. The data has uncovered important insights that can help states and hospitals better manage infection rates and patient caseloads.
The project’s website went live on March 26, less than a week after Professor of Finance Pinar Karaca-Mandic and MILI Executive in Residence Dr. Archelle Georgiou first discussed the importance of hospitalization data for modeling the disease’s impact. “There wasn’t one unified location where we or any department of health or any modelers could grab the hospitalization data,” says Georgiou, who is also a physician. “And we decided to make that happen.”
Karaca-Mandic, who also is MILI’s academic director, brought in Carlson School colleague Soumya Sen, associate professor of information and decision studies and MISRC’s academic director. Sen would help make sure project-collected data was presented in a way that it would make it useful not only to academics but also government, the media, and the general public.
Accurate Numbers, Actionable Insights
Why hospitalizations? The number of mortalities, Sen says, “is a lagging metric. It’s an important one to track. But what really matters from a decision-making perspective is the current state. How many people are actually hospitalized? And what is the impact on the hospital system as a result?”
Part of the challenge in obtaining hospitalization numbers, Karaca-Mandic notes, is that “the states varied widely on how they defined their data.” Case in point: Some states don’t separate suspected and confirmed cases. In order to get useful and verified numbers, project team members have contacted state officials, academics, and even local media.
Another challenge involved adding important new information. For instance, some states have begun reporting hospitalizations by age, gender, and racial and ethnic background. “It’s still not ideal,” Karaca- Mandic says of the data collection process. “But we’ve gotten comfortable with quickly seeing and tracking possible changes” in how states report their data.
Despite these challenges, the data has been sufficiently useful for the team to glean crucial insights. Members of the Hospitalization Project have published several papers discussing their findings:
- In May, a paper in JAMA looked at the association of stay-at-home orders with COVID-19 hospitalizations. Project data showed that 12 days after four states issued stay-at-home orders, infection trends declined, suggesting those orders had been effective.
- In August, the three project principals published a study in JAMA Internal Medicine that revealed a much higher prevalence of COVID-19 among racial and ethnic minorities than in the population as a whole.
- Also in August, a study in the Journal of General Internal Medicine examined the association of daily ICU and non-ICU use by COVID-19 patients on overall COVID-19 mortality. Early Centers for Disease Control and Prevention (CDC) data suggested that for every additional seven hospitalized patients not in ICU, there were about 0.5 additional deaths over the next seven days. The Hospitalization Project’s research, based on a larger dataset, found that the impact on the total number of COVID-19 deaths is likely higher.
More papers based on project data analysis are in the pipeline, including looking at disparate impact by age groups, rural areas, and examining multiple policy levers such as re-opening of state economies.
The Business Case for Medical Data
So why has a business school tackled a project that might seem better suited to public health or medical
school scholars?
“Healthcare is an interdisciplinary field,” Karaca-Mandic notes, and one of those disciplines is business management. The hospitalization project is “100 percent aligned” with MILI’s mission to help shape the future of the medical industry: “We identified a major data gap. This is important for policy making and for any decisions that the public health level tries to address.”
From Sen’s perspective, the project’s data work fits MISRC’s educational focus on data science and data analytics. He notes that organizations of all kinds have discovered that turning digital data into actionable insights can improve processes, anticipate future needs, and much more. “The project's data-driven approach,” Sen adds, “is widely applicable to many other organizational contexts.”


